Curriculum
Why Four Years?
Our residency thrives on innovation. Started in 1994 as the nation’s first accredited Community Health Center-sponsored Family Medicine Residency,  in 2011 the residency was designated by HRSA as one of the nation’s first 11 Teaching Health Centers under the Affordable Care Act. In May 2012, the residency was selected by the ACGME as one of 12 family medicine residencies for its national four-year length of training study, which began with the class entering in June 2013.
in 2011 the residency was designated by HRSA as one of the nation’s first 11 Teaching Health Centers under the Affordable Care Act. In May 2012, the residency was selected by the ACGME as one of 12 family medicine residencies for its national four-year length of training study, which began with the class entering in June 2013.
The mission of the LFMR is to provide residents with the skills to provide medical care and medical leadership in the emerging new healthcare system, particularly in underserved communities. Given the increasing depth of knowledge and breadth of expertise necessary for the optimal practice of Family Medicine, the addition of a fourth year of residency allows us the opportunity to provide training which offers that additional breadth and depth as well as an expanded skill set including:
- Development of competencies in all aspects of PCMH of the medical home. These include team-based care, population medicine, and community medicine in our NCQA Level 3 Family Medicine Center through immersion in and graduated responsibility for management health, information mastery, chronic disease management, practice-based improvement, and leadership.
- Increased depth of experience in core clinical aspects of Family Medicine, particularly essential in low resource clinical environments, with development of added competencies key to the care of underserved populations.
- Increased opportunity for residents to develop additional competencies in areas of personal interest through the expansion of areas of concentration (AOCs).
- More meaningful and longitudinal community experiences will serve as a foundation for substantive community involvement for residents throughout their careers.
Some Background Reading on Length of Training:
Gravel J, Rosener SE, Barr WB, Hill KJ. “Students See the Elephant” Fam Med 2019; 51(8):638-640.( https://journals.stfm.org/familymedicine/2019/september/gravel-2019-0191/)
Eiff MP, Ericson A, Uchison EW, et al. “A comparison of residency applications and match performance to 3-year versus 4-year family medicine training programs.” Fam Med. 2019;51(8):641-648 (https://journals.stfm.org/familymedicine/2019/september/eiff-2018-0542/)
Sualtz J. “Finding 8,000 Medical Students Every Year.” Fam Med 2019;51(8):633-635 (https://journals.stfm.org/familymedicine/2019/september/fte-sept-19/)
Saultz JW, David AK.”Is it Time for a 4-year Family Medicine Residency?” Fam Med 2004; 36 (5):363-6. (https://fammedarchives.blob.core.windows.net/imagesandpdfs/pdfs/FamilyMedicineVol36Issue5Saultz363.pdf)
Pugno P. “One Giant Leap for Family Medicine: Preparing the 21st-Century Physician to Practice Patient-Centered, High– Performance Family Medicine” JABFM 2010 Vol 23 Supplement (https://www.jabfm.org/content/23/Supplement/S23)
Background about Why to Extend Length of Training:
Lindbloom EJ, Ringdahl E “Resident Duty Hour Changes: Impact in the Patient-Centered Medical Home” Fam Med 2014; 46 (6):463-6. (https://www.stfm.org/familymedicine/vol46issue6/Lindbloom463)
Bazemore A, Petterson S, Peterson L, Phillips RL “More Comprehensive Care Among Family Physicians is Associated with Lower Costs and Fewer Hospitalizations” Ann Fam Med 2015;13:206-213. (https://www.annfammed.org/content/13/3/206.full)
Specific Enhancements
| INNOVATION | PURPOSE | METHOD |
| Health Systems Management (HSM) | Develop expertise in Patient-Centered Medical Home (PCMH) principles and leadership. | Longitudinal outpatient experiences in all years of curriculum. Active participation and leadership in PCMH teams. R4 Clinical Chief Block Rotation. Ongoing QI and research projects. Advocacy efforts. |
| HIV | Develop competency in providing primary care for patients with HIV. | Longitudinal outpatient experiences in team-based HIV care. |
| Addiction Medicine | Develop competency in providing primary care for patients with addiction, including in the use of buprenorphine in a primary care setting. | Continuity outpatient experiences in team-based addiction management. Standardized suboxone training and exposure to vivitrol and methadone management. |
| Behavioral Health | Develop competency to provide primary care-based mental health care and work with multi-disciplinary teams focused on behavioral and mental health. | Continuity outpatient experiences working within an integrative model. Experience with psychologists and psychiatrists in outpatient and inpatient settings, including in the VA system. |
| Care of the Underserved | Develop competencies in skills that enhance the care of underserved populations such as: health literacy, use of interpreters, care for the homeless, cross-cultural care, racism in medicine, and much more. | Integral in all areas of the curriculum. |
| Community Medicine | Develop expertise in community assessments and developing partnerships to enhance health of patients and their communities. | Didactics, community placements, partnership with community organizations, advocacy opportunities. |
| Areas of Concentration (AOC) | Develop expertise in personal area of interest. Current AOCs include: 1. Academic 2. Addiction Medicine 3. Advanced Surgical Maternity Care 4. Health Systems Leadership 5. HIV and Viral Hepatitis 6. Hospital Medicine 7. Integrative Medicine 8. Musculoskeletal Medicine 9. Reproductive and Women’s Health |
Residents are active participants in developing own learning plan and have opportunities to gain additional skills to be the “local experts” in their practice. |
| Point of Care Ultrasound (POCUS) | Develop competency to employ POCUS in a variety of outpatient and inpatient settings, including to assist in procedures. | Two-day POCUS course in R1 year. Focused experiences in ED and ICU rotations. Longitudinal experiences in continuity clinic and inpatient rotations. |
| Group Medical Visits | Residents will develop expertise in group medical visit facilitation and administration. Residents will participate in group visits in at least 2 different medical areas. | Participation as group co-facilitator (R1, R2) and lead facilitator (R3, R4) for resident clinic group visits. Current group visit models for prenatal care (Centering Pregnancy) and wellness. |
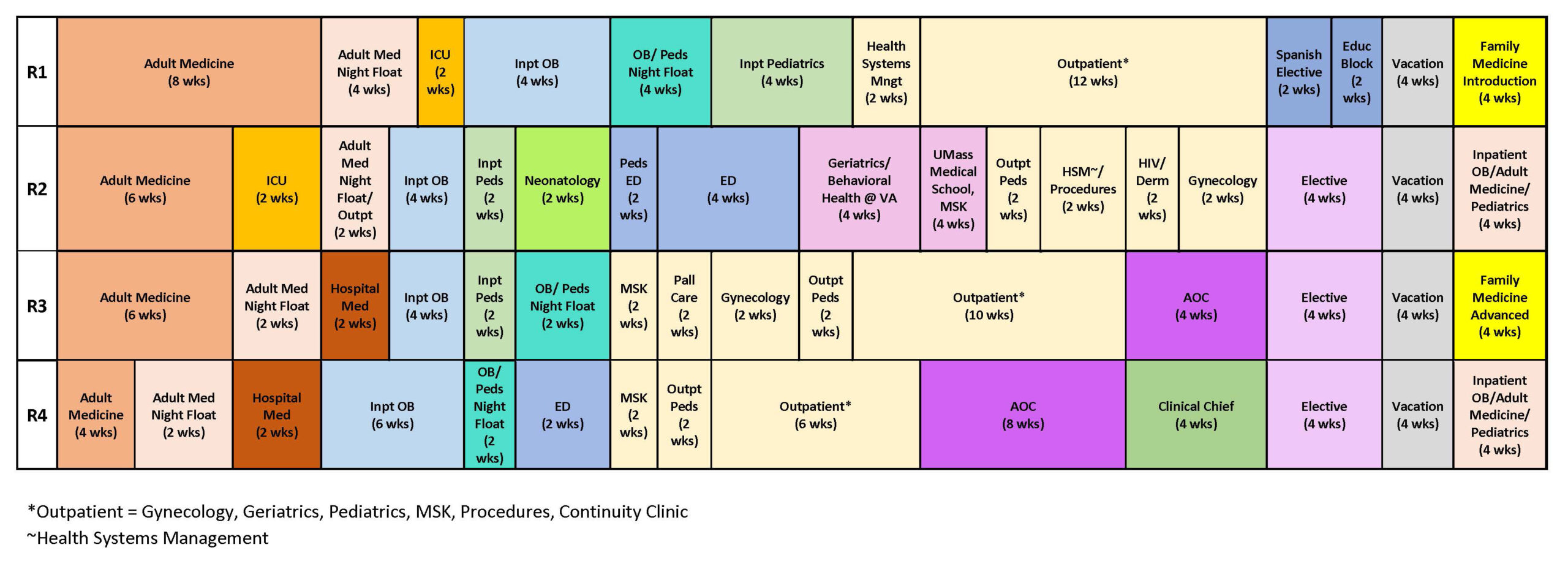
First Year Curriculum
R1 LFMR Administrative Orientation (2 weeks)
- Welcome to LFMR!
- Introduction to nuts and bolts workings of the residency and ACGME requirements.
- Orientation to software used by residency– EMRs, New Innovations, QGenda, Evernote, Greater Lawrence University (GLU), UltiPro, SharePoint, DynaMed, Epocrates – scheduling, patient care, educational support, Human Resources functions.
- Certification courses – ACLS, NRP.
- Lots of informal social events with fellow residents, faculty, staff of both GLFHC and LGH to get to know your classmates and the GLFHC/LGH community.
R1 Rassias® Spanish training (1 week) – Dartmouth College, Hanover, NH
- Entering first year class attends this 5-day course together at Dartmouth; tuition, room & board covered by residency.
- Rassias Method® is a unique approach that speeds language learning, increases language retention and has you speaking and understanding.
- Originally developed for Peace Corps training, it has been adapted by language teachers in North America, Europe, Africa and Asia.
- Instruction is individualized to meet each resident’s needs, from those with no Spanish language at program entry to those with advanced Spanish proficiency.
- For more information: http://rassias.dartmouth.edu/
R1 Introduction to Family Medicine Residency (4 weeks)
- Didactic conferences by residency faculty on common family medicine topics.
- Community medicine-introduction to community services by walking-in-our patients’- shoes “scavenger hunt”.
- Clinical care focus is orienting to clinic and hospital through seeing limited numbers of patients, meeting your patient panel and working with hospital teams and your PCMH clinical team.
- Office-based procedure workshops.
- Introduction to LFMR’s Milestones & Competency Based Evaluations.
- Basic Skills Qualifications (BSQs) teaching and testing.
R1 Adult Medicine (10 weeks)
Faculty Coordinator: Joshua St. Louis, MD, MPH
- Once weekly teaching of core topics in Adult Medicine is provided by attendings and senior residents.
- Teaching rounds, noon conferences, and Grand Rounds highlight patient problems and treatment plans and are provided by core family physician faculty, selected primary care internists, and specialists.
- There is a weekly Adult Medicine case conference presented by a resident and a faculty member.
- Sixteen patients are cared for by a team consisting of: 2-3 interns, 2 senior residents and one attending.
- Performance of common inpatient procedures is expected with direct supervision by faculty or specialists.
- Ethical issues relating to critically ill or dying patients are also addressed and coordinated with a palliative care service.
R1 Adult Medicine Night Float (2 weeks)
Faculty Coordinator: Joshua St. Louis, MD, MPH
- Teaching provided by selected family medicine and internal medicine hospitalists and specialists.
- Admissions expectations are tailored based on each resident’s inpatient experiences
- Cross coverage of daytime teaching service’s 16 patients cared for by a team consisting of: 1 first year resident and 1 senior resident and hospitalist attendings.
- Performance of common inpatient procedures is expected with direct supervision by faculty or specialists.
- Ethical issues relating to critically ill or dying patients are also addressed and coordinated with a palliative care service.
R1 Critical Care Medicine ICU (2 weeks)
Faculty Coordinator: Joshua St. Louis, MD, MPH
- Dedicated month long rotation at end of R1 year
- Assessment and management of the critically ill patient admitted to the ICU
- Teaching provided by core family physician faculty with additional critical care training and intensivist.
- Each resident cares for 3-6 patients per day
- Daily multi-disciplinary teaching rounds in ICU that includes a dedicated intensive care specialist, pharmacist, nursing.
- Core topics include: Respiratory support and ventilator management, fluid and electrolyte physiology, treatment of sepsis, use of pressors, end of life discussions.
R1 Maternity Care (4 weeks)
Faculty Coordinator: Andrew Smith, MD
- Day rotations on Labor and Delivery
- Deliveries supervised by family physicians
- Care of low- and high- risk mother-baby couplets
- Perform many vaginal deliveries including continuity patients
- Opportunity for exposure to surgical procedures such as C-sections and tubal ligations
- Daily lectures during rotation
- 2 noon-time case conferences per month
- Resident led facilitation of group prenatal visits using the CenteringPregnancy model
R1 Maternity Care/Pediatrics Night Float (4 weeks)
Faculty Coordinators: Andrew Smith, MD and Keith Nokes, MD MPH
- Night rotation on Labor and Delivery
- Extensive experience in care of hospitalized children in a community hospital setting.
- Admit ill infants and children overnight with teaching pediatric hospitalists, transfer care to inpatient pediatrics day team in morning.
- Labor & Delivery coverage in one of the busiest community hospital based Maternity units in Massachusetts.
- Maternity care supported by nearly 20 family physician attendings; 8 have C-section privileges.
- Lawrence General Hospital employs OB-GYNs dedicated to resident teaching.
R1 Hospital-Based Pediatrics (4 weeks)
Faculty Coordinator: Keith Nokes, MD MPH
- Extensive experience in care of hospitalized children in a community hospital setting.
- Co-teaching from dedicated pediatric hospitalists and family physicians.
- Academic pediatric hospitalists from Tufts’ Floating Hospital for Children in Boston.
- Focused comprehensive hospital care of infants and children.
- Rotation in Level 2 Special Care Nursery and ongoing interaction with neonatologists in pediatric and OB rotations.
- Certification in NRP and PALS for all residents.
R1 Spanish Language Elective (2 weeks)
Faculty Coordinator: Anthony Valdini, MD, MS, MPH, FACP, FAAFP
- It is neither expected nor required that entering residents speak Spanish- just willing to learn.
- In addition to the 5-day intensive Spanish Rassias course at Dartmouth College during Orientation, and individualized instruction in Lawrence throughout the year, the residency provides a supported Spanish language school experience during the R1 year for residents who do not enter resident proficient in Spanish for a second language intensive experience.
- Residents select the language school from a list of recommended overseas schools in the Caribbean, Central America, and South America.
R1 Vacation (4 weeks)
R1 Ambulatory Rotations (14 weeks):
R1 Gynecology (2 weeks)
Faculty Coordinator: Julie Johnston, MD
- Didactic training on a variety of reproductive health topics.
- Procedural workshops: IUDs, Nexplanon, Endometrial Biopsy, Uterine Aspiration, Colposcopy, and Wet Preps.
- In house Gynecology Procedural clinics with family physicians.
- One-on-one time with specialists in the clinic and operating room.
R1 Musculoskeletal (2 weeks)
Faculty Coordinator: Christie Langenberg, MD
- Develop confidence in handling common orthopedic problems encountered in the family physician’s office.
- Curriculum is complemented by formal workshops in casting and splinting, office procedures involving joint injection and aspiration.
- Fellowship-trained family physician faculty with Certification of Added Qualification in Sports Medicine.
- Area of Concentration in Sports Medicine available.
- Residents work with faculty and athletic trainers at Lawrence High School and Greater Lawrence Technical School.
- Participate in sideline medical coverage, injury clinics, rehabilitation, counseling, sport related concussion evaluation/management, pre-athletic screening services for schools, osteopathic manipulative medicine clinic, sports medicine clinics and ultrasound guided injection clinics.
- Residents also have the opportunity to volunteer as medical staff at mass participation sporting events such as triathlons and the Boston Marathon.
- Residents apply sports medicine knowledge to their patients in the Greater Lawrence Family Health Center and can elect to work as a team physician for local high school sports teams.
R1 Geriatrics (2 weeks)
Faculty Coordinator: Chelsea Harris, MD
- Longitudinal experience to acquire knowledge, attitudes and skills required for appropriate care of the elderly and principals of palliative care pertaining to the end of life & goals of care.
- Geriatrics experiences include: inpatient palliative medicine, outpatient clinic sessions dedicated to care of the elderly, core didactic lectures, home visit program
- Provide acute and continuity of care for long term residents at Mary Immaculate Nursing Home.
R1 Ambulatory Pediatrics (2 weeks)
Faculty Coordinator: Tuhin Roy, MD, MPH
- Focused experiences in ambulatory pediatrics, adolescent medicine, and developmental pediatrics.
- Lots of children in your continuity panel- 1/3rd of Lawrence’s population is under age 18.
- Extensive didactic curriculum in well child care based on Bright Horizons.
- Become familiar with common diseases and conditions of infancy, childhood, and adolescence.
- Dedicated time developing skills around infant nutrition including breastfeeding support
R1 Surgery (2 weeks)
Faculty Coordinator: John Torro, MD
- Experience in initial evaluation of patients with common surgical conditions such as abdominal pain and its differential diagnosis, inguinal hernias, management of breast disease, and colorectal malignancies in a community hospital setting, taught by community-based general surgeons.
- Outpatient procedural/surgical skillsMany performed in our own GLFHC Procedures Clinic staffed by family physician faculty.
- Focus is to learn and perform office-based surgery and to master pre- and post-operative evaluation for various surgical conditions.
- Optional additional extensive surgical training in R2-R4 years includes our Ghana global health experience led by Vince Waite, MD, a family physician faculty with additional surgical training and decades of overseas surgical experience. Residents first-assist major surgeries during this elective rotation experience.
R1 Behavioral Health (5 half-day sessions)
Faculty Coordinator: Xenia Johnson Bhembe, MD
- Prepares residents to care for the majority of their patients’ bio-psychosocial needs.
- Skill based learning taught via lectures, case conferences, support groups, Balint groups, Retreats, and dual precepting (family physician and psychologist) during continuity clinics.
- The goals of the Behavioral Medicine longitudinal experience include the following:
- Demonstrate proficiency in interpersonal skills relevant to patient care in family medicine.
- Demonstrate proficiency in the technical skills relevant to the psychosocial needs of patients in family medicine. This includes motivational interviewing, cognitive behavioral interventions as well as problem solving techniques.
- Identify and treat common psychosocial and psychiatric disorders.
- Understand those issues that interfere with forming productive doctor/patient working relationships.
R1 Integrative Medicine (5 half-day sessions)
Faculty Coordinator: Suhani Bora, MD
- Residents spend clinical sessions at our nationally- known Integrative Medicine fellowship at the GLFHC clinical site in South Lawrence.
- Exposure to modalities including acupuncture, OMT, meditation, massage therapy, group medical visits utilizing the Empowerment Model.
- Nationally known faculty member Jeff Geller, current President of IM4US, a collaborative, multidisciplinary group of people committed to affordable, accessible integrative health care for all.
R1 Community Medicine (10 half-day sessions)
Faculty Coordinators: Cara Marshall, MD and Ryan Dono, MD
- Longitudinal lectures/workshops on social medicine and public health topics
- Individual community-based placements with local organizations in area of residents’ interest
- Sessions during first year working with community health workers and local public health practitioners
- Community health education and public health advocacy integrated into AOCs
- Residents paired with Community groups such as:
- Lawrence Community Works
- Groundwork Lawrence
- YWCA
- Youth Build
- Daybreak Homeless Shelter
- Lawrence Public Library
- YMCA
- Senior Center
R1 Health Systems Management (10 half-day sessions)
Faculty Coordinator: Jonathan Lichkus, MD
- Particular emphasis placed on training residents to lead Quality Improvement efforts in their future practices.
- A goal of this curriculum is that all residents achieve Institute for Healthcare Improvement (IHI) Open School basic certification by end of R2 year.
- Develop competency in leading practice transformation, value-based care, quality improvement, advocacy, patient safety, and leadership.
- Residents choose from menu of experiential activities from specific curricular areas including performance measurement and improvement, quality and safety, community health center operations and governance, payment systems and finance, regulatory and medical-legal aspects, organizational culture and behavior, management skills and communication, leadership, care redesign and population health management, project management, health systems and policy, advocacy, data driven decision making, and personal and career management.
Point of Care Ultrasound Curriculum
- R1 Two Day Point of Care Ultrasound (POCUS) Course at LFMR – hands on experiential course with models covering all the most common POCUS exams.
- Sonosite ultrasound units (one per floor) now available in clinic for resident use.
- Ultrasounds also available for POCUS in ICU and ED in hospital.
- Focused POCUS exam goals during Maternity, ICU, and ED rotations.
- Longitudinal use encouraged in continuity clinics, sports medicine, gynecology, and procedure clinics.
- Selected family medicine faculty receiving advanced training in office-based use.
R1 Continuity Clinic (3-4 sessions/week)
Faculty Coordinators: PCMH Team Leaders
- Individual panel of patients for each resident.
- Managed within a clinical team which includes faculty advisor.
- NCQA Level 3 Patient-Centered Medical Home center.
- “Active Precepting” of all patients by family medicine faculty.
- Extensive Behavioral Science faculty staff support
- Rigorous didactic curriculum- resident-led Outpatient Ambulatory Teaching (“OAT”s) 4 times weekly on Mondays-> Thursdays and half-day Thursday afternoon conferences (“TACO”s)
R1 Spanish Longitudinal 1:1 teaching
Faculty Coordinator: Patricia Donahue and Anthony Valdini, MD, MS, MPH, FAAFP
- On site Spanish teacher/translator. A (now retired) high school Spanish teacher provides individualized lessons for residents and shadows residents in their continuity clinics for real -world instruction.
- Resident paired with bilingual medical assistant who provides language and cultural interpretation.
- Best way to learn a language is immersion (with support)- majority of daily patient interactions are in Spanish.
Second Year Curriculum
R2 Adult Medicine (4 weeks)
Faculty Coordinator: Joshua St. Louis, MD, MPH
- Teaching rounds, noon conferences, and Grand Rounds highlight patient problems and treatment plans and are provided by core family physician faculty, selected primary care internists, and specialists.
- Second year residents are in charge of supervising both pharmacy and medical students
- Residents often manage patients in critical care when on Medicine, in addition to the dedicated ICU rotation.
- Sixteen patients are cared for by a team consisting of: 2-3 interns, 2 senior residents and one attending.
- Performance of common inpatient procedures is expected with direct supervision by faculty or specialists.
- Ethical issues relating to critically ill or dying patients are also addressed and coordinated with a palliative care service.
R2 Adult Medicine Night Float (4 weeks)
Faculty Coordinator: Joshua St. Louis, MD, MPH
- Teaching provided by selected family medicine and internal medicine hospitalists and specialists.
- Senior residents supervise interns in admissions and management of floor issues
- Cross coverage of daytime teaching service’s 16 patients cared for by a team consisting of: usually1 first year resident and 1 senior resident and hospitalist attendings.
- Performance of common inpatient procedures is expected with direct supervision by faculty or specialists.
- Ethical issues relating to critically ill or dying patients are also addressed and coordinated with a palliative care service.
R2 Critical Care Medicine ICU2 (2 weeks)
Faculty Coordinator: Joshua St. Louis, MD, MPH
- Teaching provided by intensivist along with adult medicine family medicine attending.
- Each resident cares for 3-5 critically patients per day.
- Day time only rotation – integrated with larger medicine team to cover resident patients at night and on day off.
- Daily multi-disciplinary teaching rounds in ICU that includes a dedicated intensive care specialist, pharmacist, nursing.
- Opportunities to gain more inpatient procedural experiences (including central lines, POCUS exams, etc.).
R2 Maternity Care (4 weeks)
Faculty Coordinator: Andrew Smith, MD
- Day rotation on Labor and Delivery and postpartum
- Deliveries supervised by family physicians
- Care of low- and high- risk mother-baby couplets
- Perform many vaginal deliveries including continuity patients
- Opportunity for exposure to surgical procedures such as C-sections and tubal ligations
- Daily lectures during rotation
- 2 noon-time case conferences per month
- Resident led facilitation of group prenatal visits using the CenteringPregnancy model
R2 Pediatrics Emergency Department (2 weeks)
Faculty Coordinator: Keith Nokes, MD MPH
- Rotation in busy Pediatric Emergency Department.
- Paired with dedicated emergency pediatrician faculty.
- High volume, hands-on experience.
- Numerous opportunities for procedures.
R2 Pediatrics – Swing (2 weeks)
Faculty Coordinator: Keith Nokes, MD MPH
- Extensive experience in care of hospitalized children in a community hospital setting.
- Co-teaching from dedicated pediatric hospitalists and family physicians.
- Academic pediatric hospitalists from Tufts’ Floating Hospital for Children in Boston.
- Focused comprehensive hospital care of infants and children.
- Rotation in Level 2 Special Care Nursery and ongoing interaction with neonatologists in pediatric and OB rotations.
- Certification in NRP and PALS for all residents.
R2 Geriatrics Bedford VA (2 weeks)
Faculty Coordinator: Chelsea Harris, MD
- 2-week block experience at the VA hospital in Bedford, MA, on their GEM (Geriatric Evaluation and Management) Unit, which provides inpatient rehabilitation and respite care as well as outpatient geriatric services.
- Experiential and didactic learning around comprehensive multi-disciplinary evaluation of geriatric patients.
- Focus on functional assessment, decreasing polypharmacy, fall prevention, goals of care, geriatric pharmacology, assistive devices, incontinence and supportive services to maintain independence.
R2 Neonatology (2 weeks)
Faculty Coordinator: Keith Nokes, MD MPH
- Rotation in busy LGH Level 2 Neonatal Nursery.
- Residents develop a systematic approach to the initial evaluation, diagnosis and management of common neonatal problems such as respiratory distress, apnea, hypoglycemia, seizures, sepsis, jaundice, prematurity, opiate withdrawal, growth disorders, fluid balance, etc.
- Residents learn to competently perform neonatal resuscitation.
- Residents learn procedures such as venipuncture, IV placement, LPs.
- Identify core issues for primary care physician follow-up after baby discharged.
R2 Emergency Medicine (4 weeks)
Faculty Coordinator: John Torro, MD
- Rotate at Lawrence General Hospital Emergency Department.
- Paired with emergency medicine staff physicians and benefit from one-on-one teaching and high-volume, hands-on experience.
- Residents learn to perform common emergency department procedures such as suturing, NG Tube placement, IV insertion, and intubation.
- Opportunities to learn point of care ultrasound.
- Lawrence General Hospital’s 41 bay Emergency Department is one of the busiest in Massachusetts (73,000 visits annually)
- LGH Emergency Department is a designated Level III trauma center.
R2 Elective (4 weeks)
Faculty Coordinators: Faculty Advisors
- Numerous elective rotations available with specialist, community, primary care resources.
- Global Health electives with LFMR family physician faculty.
R2 Vacation (4 weeks)
R2 Ambulatory Rotations (20 weeks):
R2 Gynecology (2 weeks)
Faculty Coordinator: Julie Johnston, MD
- Training in a variety of reproductive health topics.
- Procedural workshops: IUDs, Nexplanon, Endometrial Biopsy, Uterine Aspiration, Colposcopy, and Wet Preps.
- In house Gynecology Procedural clinics with Family physicians.
- One-on-one time with specialists in the clinic and operating room.
R2 Musculoskeletal (2 weeks)
Faculty Coordinator: Christie Langenberg, MD
- Develop confidence in handling common orthopedic problems encountered in the family physician’s office.
- Curriculum is complemented by formal workshops in casting and splinting, office procedures involving joint injection and aspiration.
- Fellowship-trained family physician faculty with Certification of Added Qualification in Sports Medicine.
- Area of Concentration in Sports Medicine available.
- Residents work with faculty and athletic trainers at Lawrence High School and Greater Lawrence Technical School.
- Participate in sideline medical coverage, injury clinics, rehabilitation, counseling, sport related concussion evaluation/management, pre-athletic screening services for schools, osteopathic manipulative medicine clinic, sports medicine clinics and ultrasound guided injection clinics.
- Residents also have the opportunity to volunteer as medical staff at mass participation sporting events such as triathlons and the Boston Marathon.
- Residents apply sports medicine knowledge to their patients in the Greater Lawrence Family Health Center and can elect to work as a team physician for local high school sports teams.
R2: Ambulatory Pediatrics (2 weeks)
Faculty Coordinator: : Tuhin Roy, MD, MPH
- Focused experiences in ambulatory pediatrics and adolescent medicine.
- Develop skills around failure to thrive, growth and nutrition in childhood.
- Dedicated time developing skills around infant nutrition including breastfeeding support.
R2 HIV Medicine (2 weeks)
Faculty Coordinators: Katrina Baumgartner, MD and Joshua St. Louis, MD, MPH
- Residents will see patients with HIV specialist family medicine physicians in multidisciplinary team-based clinic settings.
- Residents will gain experience in:
- Evidence-based prevention interventions for HIV and viral hepatitis, including:
- Pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP)
- Obtaining a sexual health history, and screening and treatment of STIs
- Screening and treatment of substance use disorders
- Primary care management of persons living with HIV
- Basic antiretroviral therapy (ART) management, including monitoring for and identification of common ART complications
- Prevention and management of common infectious and non-infectious complications of HIV
- Screening, diagnosis and treatment of hepatitis C and hepatitis B infections
- Utilization of available HIV- and viral-hepatitis-related resources, within and outside the clinic, to optimize patient care
- Evidence-based prevention interventions for HIV and viral hepatitis, including:
- An Area of Concentration in HIV Medicine leading to HIV specialist certification is available.
R2 Dermatology (2 weeks)
Faculty Coordinator: Ryan Dono, MD
- Residents learn evaluation and management of skin conditions affecting our multiracial patient population.
- Work directly with board-certified dermatologists.
- Learn office-based skin procedures, particularly important for FPs caring for underserved patient populations with relatively limited access to general dermatologist services in most socioeconomically disadvantaged communities.
R2 Behavioral Health (5 half-day sessions)
Faculty Coordinatos: Xenia Johnson Bhembe, MD
- Prepares residents to care for the majority of their patients’ bio-psychosocial needs.
- Skill based learning taught via lectures, case conferences, support groups, Balint groups, Retreats, and dual precepting (family physician and psychologist) during continuity clinics.
- The goals of the Behavioral Medicine longitudinal experience include the following:
- Demonstrate proficiency in interpersonal skills relevant to patient care in family medicine.
- Demonstrate proficiency in the technical skills relevant to the psychosocial needs of patients in family medicine. This includes motivational interviewing, cognitive behavioral interventions as well as problem solving techniques.
- Identify and treat common psychosocial and psychiatric disorders.
- Understand those issues that interfere with forming productive doctor/patient working relationships.
R2 Integrative Medicine (5 half day sessions)
Faculty Coordinator: Suhani Bora, MD
- Residents spend clinical sessions at our nationally- known Integrative Medicine fellowship at the GLFHC clinical site in South Lawrence.
- Exposure to modalities including acupuncture, OMT, meditation, massage therapy, group medical visits utilizing the Empowerment Model.
R2 Addiction Medicine (5 half-day sessions)
Faculty Coordinator: Steven Buttenwieser, MD
- Residents obtain significant experience caring for patients with addictions.
- All residents complete Buprenorphine / Naloxone (Suboxone) training and certification prior to graduation.
- GLFHC Suboxone program has over 400 active patients, residents precepted by family physicians with special expertise in addiction medicine.
- Learn screening, diagnosis, evaluation and treatment of addiction disorders including medication, non-pharmacologic modalities, counseling, and psychosocial/spiritual approaches.
- Proper use and interpretation of office-based toxicity screens.
- Appropriate use of opiates in clinical practice and best practices including systems processes.
- Use of Naloxone in public health and as overuse antidote in community.
R2 Medical and Surgical Subspecialties (5 half-day sessions)
Faculty Coordinator: Cara Marshall, MD
- One-on-one rotation time with subspecialists; focused on ENT, Ophthalmology, & Urology.
- Longitudinal interactive primary-care focused didactic curriculum.
- Extensive continuity panel experience.
- Dedicated Procedure clinics for intensive procedure training.
R2 Community Medicine (10 half-day sessions)
Faculty Coordinators: Cara Marshall, MD and Ryan Dono, MD
- Longitudinal lectures/workshops on social medicine and public health topics.
- Individual community-based placements with local organizations in area of residents’ interest.
- Community health education and public health advocacy integrated into AOCs.
- Residents paired with Community groups such as:
- Lawrence Community Works
- Groundwork Lawrence
- YWCA
- Youth Build
- Daybreak Homeless Shelter
- Lawrence Public Library
- YMCA
- Senior Center
R2 Behavioral Health Bedford VA (2 weeks)
Faculty Coordinators: Jenni Somers, MD and Cara Marshall, MD
- Block rotation at the PCBH (Primary Care Behavioral Health) department at the VA hospital in Bedford, MA, including inpatient and outpatient psychiatric/behavioral health care of veterans. Prepares residents to care for the majority of their patients’ bio-psychosocial needs.
- The goals of the Behavioral Medicine experience include the following:
- Demonstrate proficiency in interpersonal skills relevant to patient care in family medicine.
- Demonstrate proficiency in the technical skills relevant to the psychosocial needs of patients in family medicine. This includes motivational interviewing, cognitive behavioral interventions as well as problem solving techniques.
- Identify and treat common psychosocial and psychiatric disorders.
- Understand those issues that interfere with forming productive doctor/patient working relationships.
R2 Health Systems Management (10 half-day sessions)
Faculty Coordinator: Jonathan Lichkus, MD
- Particular emphasis placed on training residents to lead Quality Improvement efforts in their future practices.
- A goal of this curriculum is that all residents achieve Institute for Healthcare Improvement (IHI) Open School basic certification by end of R2 year.
- Develop competency in leading practice transformation, value-based care, quality improvement, advocacy, patient safety, and leadership
- Residents choose from menu of experiential activities from specific curricular areas including performance measurement and improvement, quality and safety, community health center operations and governance, payment systems and finance, regulatory and medical-legal aspects, organizational culture and behavior, management skills and communication, leadership, care redesign and population health management, project management, health systems and policy, advocacy, data driven decision making, and personal and career management.
Point of Care Ultrasound Curriculum
- Sonosite ultrasound units (one per floor) now available in clinic for resident use.
- Ultrasounds also available for POCUS in ICU and ED in hospital.
- Focused POCUS exam goals during Maternity, ICU, and ED rotations.
- Longitudinal use encouraged in continuity clinics, sports medicine, gynecology, and procedure clinics.
- Selected family medicine faculty receiving advanced training in office-based use.
R2 Continuity Clinic (4-5 half-day sessions/week)
Faculty Coordinators: PCMH Team Leaders
- Individual panel of patients for each resident.
- Managed within a clinical team which includes faculty advisor.
- NCQA Level 3 Patient-Centered Medical Home center.
- “Active Precepting” of all patients by family medicine faculty.
- Extensive Behavioral Science faculty staff support.
- Rigorous didactic curriculum- resident-led Outpatient Ambulatory Teaching (“OAT”s) 4 times weekly on Mondays-> Thursdays and half-day Thursday afternoon conferences (“TACO”s).
Note: Resident’s Area of Concentration is selected in second half of R2 year.
Faculty Coordinators: Faculty Advisors and AOC Advisors
- 9 different Area of Concentration options are offered to LFMR residents.
- Select Area of Concentration, meet with Faculty Advisor and AOC Advisor.
- Start planning AOC-related QI and Scholarly activity projects.
View our webpage for Area of Concentration descriptions and more information.
Third Year Curriculum
R3 Family Medicine Advanced Skills (4 weeks)
Faculty Coordinator: Tuhin Roy, MD, MPH
- Focused didactic curriculum on advanced clinical topics such as: chronic pain, osteopathic manipulation, population health, academic research and scholarly work, and implicit bias training.
R3 Adult Medicine (2 weeks)
Faculty Coordinator: Joshua St. Louis, MD, MPH
- Teaching rounds, noon conferences, and Grand Rounds highlight patient problems and treatment plans and are provided by core family physician faculty, selected primary care internists, and specialists.
- Third year resident’s role will vary depending on the composition of the team
- Residents often manage patients in critical care when on Medicine, in addition to the dedicated ICU rotation.
- Sixteen patients are cared for by a team consisting of: 2 interns, 2 senior residents and one attending.
- Performance of common inpatient procedures is expected with direct supervision by faculty or specialists.
- Ethical issues relating to critically ill or dying patients are also addressed and coordinated with a palliative care service.
R3 Adult Medicine Night Float (2 weeks)
Faculty Coordinator: Joshua St. Louis, MD, MPH
- Teaching provided by selected family medicine and internal medicine hospitalists and specialists.
- Senior residents supervise interns in admissions and management of floor issues
- Cross coverage of daytime teaching service’s 16 patients cared for by a team consisting of: usually 1 first year resident and 1 senior resident and hospitalist attendings.
- Performance of common inpatient procedures is expected with direct supervision by faculty or specialists.
- Ethical issues relating to critically ill or dying patients are also addressed and coordinated with a palliative care service.
R3 HMED (Hospital Medicine): 2 weeks
Faculty Coordinator: Jennifer Somers, MD
- Hospital coverage rotation
- First-call for hospital coverage in events of resident call-out or high patient volume
- First-call for outpatient specialty clinic coverage in events of resident call-out or high patient volume
- Distance learning, project time, and clinics scheduled if not needed for hospital/specialty clinic coverage
R3 Maternity Care (4-6 weeks)
Faculty Coordinator: Andrew Smith, MD
- Day rotations on Labor and Delivery at both Lawrence General and Holy Family Hospitals.
- Most deliveries supervised by family physicians.
- Care of low- and high- risk mother-baby couplets.
- Perform many vaginal deliveries including continuity patients.
- Opportunity for exposure to surgical procedures such as C-sections and tubal ligations a Lawrence General Hospital.
- Daily lectures during rotation.
- 2 noon-time case conferences per month.
- Resident-led facilitation of group prenatal visits using the CenteringPregnancy model.
R3 Maternity Care/Pediatrics Night Float (2 weeks)
Faculty Coordinators: Andrew Smith, MD and Keith Nokes, MD MPH
- Night Rotation on Labor and Delivery
- Extensive experience in care of hospitalized children in a community hospital setting.
- Admit ill infants and children overnight with teaching pediatric hospitalists, transfer care to inpatient pediatrics day team in morning.
- Labor & Delivery coverage in one of the busiest community hospital based Maternity units in Massachusetts.
- Maternity care supported by nearly 20 family physician attendings; 8 have C-section privileges.
- Lawrence General Hospital employs OB-GYNs dedicated to resident teaching.
R3 Palliative Care (2 weeks)
Faculty Coordinator: Chelsea Harris, MD
- Longitudinal experience to acquire knowledge, attitudes and skills required for appropriate care of the elderly and principals of palliative care pertaining to the end of life & goals of care.
- Geriatrics experiences include: inpatient palliative medicine, outpatient clinic sessions dedicated to care of the elderly, core didactic lectures, home visit program.
- Provide acute and continuity of care for long term residents at Mary Immaculate Nursing Home.
R3 Surgery (2 weeks)
Faculty Coordinator: John Torro, MD
- Experience in initial evaluation of patients with common surgical conditions such as abdominal pain and its differential diagnosis, inguinal hernias, management of breast disease, and colorectal malignancies in a community hospital setting, taught by community-based general surgeons.
- Outpatient procedural/surgical skills Many performed in our own GLFHC Procedures Clinic staffed by family physician faculty.
- Focus is to learn and perform office-based surgery and to master pre- and post-operative evaluation for various surgical conditions.
- Optional additional extensive surgical training in R2-R4 years includes our Ghana global health experience led by Vince Waite, MD, a family physician faculty with additional surgical training and decades of overseas surgical experience. Residents first-assist major surgeries during this elective rotation experience.
R3 Pediatrics – Hospital-Based (4 weeks)
Faculty Coordinator: Keith Nokes, MD MPH
- Extensive experience in care of hospitalized children in a community hospital setting.
- Co-teaching from dedicated pediatric hospitalists and family physicians.
- Focused pediatric emergency care admissions from busy Emergency Department.
- Ongoing interaction with neonatologists in pediatric and maternity care rotations.
- Certification in NRP and PALS for all residents.
R3 Sports Medicine (4 weeks)
Faculty Coordinator: Christie Langenberg, MD
- See patients with Sports Medicine family physicians, emphasizing an office setting.
- Develop confidence in handling common orthopedic and sports medicine problems encountered in the family physician’s office.
- Curriculum is complemented by formal workshops in casting and splinting, office procedures involving joint injection and aspiration.
- Fellowship-trained family physician faculty with Certification of Added Qualification in Sports Medicine.
- Area of Concentration in Sports Medicine available.
- Residents work with faculty and athletic trainers at Lawrence High School and Greater Lawrence Technical School.
- Participate in sideline medical coverage, injury clinics, rehabilitation, counseling, sport related concussion evaluation/management, pre-athletic screening services for schools, osteopathic manipulative medicine clinic, sports medicine clinics and ultrasound guided injection clinics.
- Residents also have the opportunity to volunteer as medical staff at mass participation sporting events such as triathlons and the Boston Marathon.
- Residents apply sports medicine knowledge to their patients in the Greater Lawrence Family Health Center and can elect to work as a team physician for local high school sports teams.
R3 Elective/ Area of Concentration (8 weeks)
Faculty Coordinators: Faculty Advisors and AOC Advisors
- 9 different Area of Concentration options are offered to LFMR residents.
- Continue work on Area of Concentration, meet regularly with AOC Advisor.
- Serve as your AOC’s AOC (Ambassador of Consultation) for fellow residents and faculty for clinical questions that arise in resident’s Area of Concentration.
- Work on AOC-related QI and Scholarly activity projects.
View our webpage for Area of Concentration descriptions and more information.
R3 Vacation (4 weeks)
R3 Ambulatory Rotations (20 weeks):
R3 Gynecology (2 weeks)
Faculty Coordinator: Julie Johnston, MD
- Training in a variety of reproductive health topics.
- Procedural workshops: IUDs, Nexplanon, Endometrial Biopsy, Uterine Aspiration, Colposcopy, and Wet Preps.
- In house Gynecology Procedural clinics with Family physicians.
- One-on-one time with specialists in the clinic and operating room.
R3: Ambulatory Pediatrics (4 weeks)
Faculty Coordinator: Tuhin Roy, MD, MPH
- Specialty Pediatrics exposures.
- Focused experiences in ambulatory pediatrics and adolescent medicine.
- Dedicated time developing skills around infant nutrition including breastfeeding support.
R3 Community Medicine (10 half-day sessions)
Faculty Coordinators: Cara Marshall, MD and Ryan Dono, MD
- Longitudinal lectures/workshops on social medicine and public health topics.
- Individual community-based placements with local organizations in area of residents’ interest.
- Community health education and public health advocacy integrated into AOCs.
- Residents paired with Community groups such as:
- Lawrence Community Works
- Groundwork Lawrence
- YWCA
- Youth Build
- Daybreak Homeless Shelter
- Lawrence Public Library
- YMCA
- Senior Center
R3 Health Systems Management (10 half-day sessions)
Faculty Coordinator: Jonathan Lichkus, MD
- Particular emphasis placed on training residents to lead Quality Improvement efforts in their future practices.
- A goal of this curriculum is that all residents achieve Institute for Healthcare Improvement (IHI) Open School basic certification by end of R2 year.
- Develop competency in leading practice transformation, value-based care, quality improvement, advocacy, patient safety, and leadership.
- Residents choose from menu of experiential activities from specific curricular areas including performance measurement and improvement, quality and safety, community health center operations and governance, payment systems and finance, regulatory and medical-legal aspects, organizational culture and behavior, management skills and communication, leadership, care redesign and population health management, project management, health systems and policy, advocacy, data driven decision making, and personal and career management.
R3 Continuity Clinic (4-5 half-day sessions/week)
Faculty Coordinators: PCMH Team Leaders
- Individual panel of patients for each resident.
- Managed within a clinical team which includes faculty advisor.
- NCQA Level 3 Patient-Centered Medical Home center.
- “Active Precepting” of all patients by family medicine faculty.
- Extensive Behavioral Science faculty staff support.
- Rigorous didactic curriculum- resident-led Outpatient Ambulatory Teaching (“OAT”s) 4 times weekly on Mondays-> Thursdays and half-day Thursday afternoon conferences (“TACO”s).
Point of Care Ultrasound Curriculum
- Sonosite ultrasound units (one per floor) now available in clinic for resident use.
- Ultrasounds also available for POCUS in ICU and ED in hospital.
- Focused POCUS exam goals during Maternity, ICU, and ED rotations.
- Longitudinal use encouraged in continuity clinics, sports medicine, gynecology, and procedure clinics.
- Selected family medicine faculty receiving advanced training in office-based use.
Fourth Year Curriculum
R4 Adult Medicine (4 weeks)
Faculty Coordinator: Joshua St. Louis, MD, MPH
- Teaching rounds, noon conferences, and Grand Rounds highlight patient problems and treatment plans and are provided by core family physician faculty, selected primary care internists, and specialists.
- Fourth year residents manage the Adult Medicine team and function as teacher and overseer of the entire service with a specific focus on support of interns
- Residents often manage patients in critical care when on Medicine, in addition to the dedicated ICU rotation.
- Sixteen patients are cared for by a team consisting of: 2-3 interns, 2 senior residents and one attending.
- Performance of common inpatient procedures is expected with direct supervision by faculty or specialists.
- Ethical issues relating to critically ill or dying patients are also addressed and coordinated with a palliative care service.
R3 HMED – Hospital Medicine (2 weeks)
Faculty Coordinator: Jennifer Somers, MD
- Hospital coverage rotation.
- First-call for hospital coverage in events of resident call-out or high patient volume.
- First-call for outpatient specialty clinic coverage in events of resident call-out or high patient volume.
- Distance learning, project time, and clinics scheduled if not needed for hospital/specialty clinic coverage.
R4 Clinical Chief (4-6 weeks)
Faculty Coordinator: Jonathan Lichkus, MD
- R4 resident serves as Haverhill Street “Clinical Chief”, working closely with residency clinical site’s Medical Director, Site Operations Director, and staff on all facets of running a CHC practice.
- Nuts and bolts management of clinic and leadership skills put into practice, with faculty mentorship.
- Specific required activities and optional activities selected from menu of choices.
- Quality improvement on clinic-wide basis emphasized.
- Participation in system-wide Quality Council and other clinic leadership meetings.
- Integrates previous Health Systems Management learning into a “capstone” management and leadership experience.
R4 Maternity Care (4 weeks)
Faculty Coordinator: Andrew Smith, MD
- Day rotations on Labor and Delivery at both Lawrence General and Holy Family Hospitals.
- Most deliveries supervised by family physicians.
- Care of low- and high- risk mother-baby couplets.
- Perform many vaginal deliveries including continuity patients.
- Opportunity for exposure to surgical procedures such as C-sections and tubal ligations a Lawrence General Hospital.
- Daily lectures during rotation.
- 2 noon-time case conferences per month.
- Resident-led facilitation of group prenatal visits using the CenteringPregnancy model.
R4 Maternity Care/Pediatrics Night Float (2 weeks)
Faculty Coordinators: Andrew Smith, MD and Keith Nokes, MD MPH
- Night Rotation on Labor and Delivery.
- Extensive experience in care of hospitalized children in a community hospital setting.
- Admit ill infants and children overnight with teaching pediatric hospitalists, transfer care to inpatient pediatrics day team in morning.
- Labor & Delivery coverage in one of the busiest community hospital based Maternity units in Massachusetts.
- Maternity care supported by nearly 20 family physician attendings; 8 have C-section privileges.
- Lawrence General Hospital employs OB-GYNs dedicated to resident teaching.
R4 Pediatric Emergency Department (2 weeks)
Faculty Coordinator: Keith Nokes, MD MPH
- Rotation in busy Pediatric Emergency Department at Lawrence General Hospital.
- Paired with dedicated emergency pediatrician faculty.
- High volume, hands-on experience.
- Procedure-rich rotation.
R4 Surgery (2 weeks)
Faculty Coordinator: John Torro, MD
- Experience in initial evaluation of patients with common surgical conditions such as abdominal pain and its differential diagnosis, inguinal hernias, management of breast disease, and colorectal malignancies in a community hospital setting, taught by community-based general surgeons.
- Outpatient procedural/surgical skills Many performed in our own GLFHC Procedures Clinic staffed by family physician faculty.
- Focus is to learn and perform office-based surgery and to master pre- and post-operative evaluation for various surgical conditions.
- Optional additional extensive surgical training in R2-R4 years includes our Ghana global health experience led by Vince Waite, MD, a family physician faculty with additional surgical training and decades of overseas surgical experience. Residents first-assist major surgeries during this elective rotation experience.
R4 Emergency Medicine (2 weeks)
Faculty Coordinator: John Torro, MD
- Rotate at Lawrence General Hospital Emergency Department.
- Paired with emergency medicine staff physicians and benefit from one-on-one teaching and high-volume, hands-on experience.
- Residents learn to perform common emergency department procedures such as suturing, NG Tube placement, IV insertion, and intubation.
- Opportunities to learn point of care ultrasound.
- Lawrence General Hospital’s 41 bay Emergency Department is one of the busiest in Massachusetts (73,000 visits annually).
- LGH Emergency Department is a designated Level III trauma center.
R4 Area of Concentration (8 weeks)
Faculty Coordinators: AOC Advisors
- 9 different Area of Concentration options are offered to LFMR residents.
- Continue work on Area of Concentration, complete requirements this year.
- Serve as your AOC’s AOC (Ambassador of Consultation) for fellow residents and faculty for clinical questions that arise in resident’s Area of Concentration.
- Complete AOC-related QI and Scholarly activity projects.
View our webpage for Area of Concentration descriptions and more information.
R4 Elective (4 weeks)
Faculty Coordinators: Faculty Advisors
- Residents choose elective experience based upon their learning needs and interests, distinct from their chosen Area of Concentration.
- This time often used for additional Global Health educational experiences.
- Additional work in Community academic projects, scholarly activity.
- Residency’s location in “medically dense” Boston metropolitan area offers many elective options including specialists at Lawrence General Hospital and our other affiliated hospitals Tufts Medical Center, University of Massachusetts Medical Center, and Beth-Israel Deaconess Medical Center in Boston.
R4 Vacation (4 weeks)
R4 Ambulatory Rotations (16 weeks):
R4 Musculoskeletal (2 weeks)
Faculty Coordinator: Christie Langenberg, MD
- Develop confidence in handling common orthopedic problems encountered in the family physician’s office.
- Curriculum is complemented by formal workshops in casting and splinting, office procedures involving joint injection and aspiration.
- Fellowship-trained family physician faculty with Certification of Added Qualification in Sports Medicine.
- Area of Concentration in Sports Medicine available.
- Residents work with faculty and athletic trainers at Lawrence High School and Greater Lawrence Technical School.
- Participate in sideline medical coverage, injury clinics, rehabilitation, counseling, sport related concussion evaluation/management, pre-athletic screening services for schools, osteopathic manipulative medicine clinic, sports medicine clinics and ultrasound guided injection clinics.
- Residents also have the opportunity to volunteer as medical staff at mass participation sporting events such as triathlons and the Boston Marathon.
- Residents apply sports medicine knowledge to their patients in the Greater Lawrence Family Health Center and can elect to work as a team physician for local high school sports teams.
R4: Ambulatory Pediatrics (2 weeks)
Faculty Coordinator: Tuhin Roy, MD, MPH
- Focused experiences in ambulatory pediatrics, adolescent medicine, and developmental pediatrics.
- Specialty Pediatrics exposures.
R4 Community Medicine (10 half-day sessions)
Faculty Coordinators: Cara Marshall, MD and Ryan Dono, MD
- Longitudinal lectures/workshops on social medicine and public health topics.
- Individual community-based placements with local organizations in area of residents’ interest.
- Community health education and public health advocacy integrated into AOCs.
- Residents paired with Community groups such as:
- Lawrence Community Works
- Groundwork Lawrence
- YWCA
- Youth Build
- Daybreak Homeless Shelter
- Lawrence Public Library
- YMCA
- Senior Center
R4 Health Systems Management (10 half-day sessions)
Faculty Coordinator: Jonathan Lichkus, MD
- Particular emphasis placed on training residents to lead Quality Improvement efforts in their future practices.
- A goal of this curriculum is that all residents achieve Institute for Healthcare Improvement (IHI) Open School basic certification by end of R2 year.
- Develop competency in leading practice transformation, value-based care, quality improvement, advocacy, patient safety, and leadership.
- Residents choose from menu of experiential activities from specific curricular areas including performance measurement and improvement, quality and safety, community health center operations and governance, payment systems and finance, regulatory and medical-legal aspects, organizational culture and behavior, management skills and communication, leadership, care redesign and population health management, project management, health systems and policy, advocacy, data driven decision making, and personal and career management.
R4 Medical and Surgical Subspecialties (5 half-day sessions)
Faculty Coordinator: Cara Marshall, MD
- One-on-one rotation time with subspecialists; focused on ENT, Ophthalmology, & Urology.
- Longitudinal interactive primary-care focused didactic curriculum.
- Extensive continuity panel experience.
- Dedicated Procedure clinics for intensive procedure training.
Point of Care Ultrasound Curriculum
- Sonosite ultrasound units (one per floor) now available in clinic for resident use.
- Ultrasounds also available for POCUS in ICU and ED in hospital.
- Focused POCUS exam goals during Maternity, ICU, and ED rotations.
- Longitudinal use encouraged in continuity clinics, sports medicine, gynecology, and procedure clinics.
- Selected family medicine faculty receiving advanced training in office-based use.
R4 Continuity Clinic (4-5 half-day sessions/week)
Faculty Coordinators: PCMH Team Leaders
- Individual panel of patients for each resident.
- Managed within a clinical team which includes faculty advisor.
- NCQA Level 3 Patient-Centered Medical Home center.
- “Active Precepting” of all patients by family medicine faculty.
- Extensive Behavioral Science faculty staff support.
- Rigorous didactic curriculum- resident-led Outpatient Ambulatory Teaching (“OAT”s) 4 times weekly on Mondays-> Thursdays and half-day Thursday afternoon conferences (“TACO”s).